Dr. Robert Pastore, PhD, CNS
Refractory Celiac Disease
2020-05-23 • 5 min read
Refractory celiac disease is identical to celiac disease except that in refractory celiac disease the patient is unresponsive to at least 1 year of treatment with a strict gluten free diet and they receive the diagnosis only after a thorough examination.
How is it diagnosed?
It is my opinion that it must be evaluated as part of the diagnostic process, so I guess you could say in my view it is diagnosed by the process of elimination and a thorough medical examination.
- First, you need to review the original diagnosis of celiac disease, going back as far as you can to in the medical records, including the original biopsy, serology, DNA, etc., and then you must have confirmation that the patient was following a strict GF diet for at least 1 year but still has symptoms and villi damage. You want to be certain there is no gluten contamination because that could rule out RCD quickly.
- Next, you double down on identifying any other condition that can negatively impact the villi including cancers such as intestinal lymphoma, inflammatory bowel disease such as Crohn’s disease, microscopic colitis, hypogammaglobulinemia (is an immune system abnormality that results in reduced antibody production making enough antibodies called immunoglobulins) and believe it or not, even small intestinal bacterial overgrowth – if severe enough, over use of NSAIDS or reaction to NSAIDS, etc.
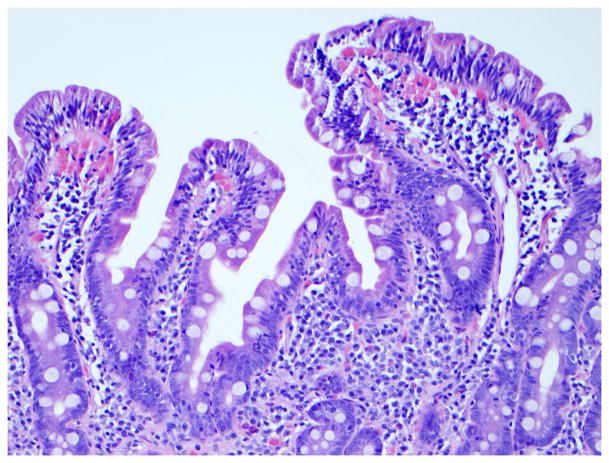
- Then, an endoscopy and colonoscopy must be performed, with biopsies taken at both sites.
- In a perfect world I like a capsule endoscopy which is basically swallowing a camera in a pill format. You can obtain excellent images and identify some inflammation and ulceration.
- Also, it may warranted to have a CT scan (computerized tomography) and MRE (Magnetic resonance enterography) as well as a barium x-ray (A barium X-ray is a radiographic (X-ray) examination of the gastrointestinal (GI) tract. Barium absorbs x-rays and appears white on the images. These tests should be done particularly if there is any suspicion of lymphoma. There may be multiple diagnoses during the search for the cause behind suspected refractory celiac disease.
- Finally, fecal fat and pancreatic tests should be completed as well.
Types of Refractory Celiac Disease
There are two types. Type 1 which has a better prognosis than type 2 which is very high risk for lymphoma. Type 1 is characterized by normal intestinal epithelial lymphocytes and type 2 with abnormal or premalignant lymphocytes (they are immature and precancerous). In type 2 malnutrition risk is extremely high. Some data indicates 85% of refractory celiac disease patients have type 1. So type 2 is the minority by far.
What is the prevalence of refractory celiac disease within the celiac disease population?
Currently it is 1 to 2% of diagnosed celiac disease patients. Interestingly enough, the individuals that present with this rare type of celiac disease are typically over 50 years of age.
What are the signs and symptoms?
The challenge for even the knowledgeable physician is that the symptoms are virtually identical to celiac disease except they are typically more severe.
Is there any physical difference between refractory celiac disease and celiac disease?
In some refractory celiac disease patients there have been reports of ulceration of the middle part of the small intestine called the jejunum which is called ulcerative jejunitis. This is quite serious because if this is present there is a high risk of what is known as enteropathy associated T cell lymphoma.
What are the causes of refractory celiac disease?
Sadly, we are not sure. We know what goes wrong. In celiac disease the T cells that are so aggressive against gliadin and that are involved in the pathology become inactive on a strict GF diet. In refractory celiac disease the intestinal T cells are still active even with gluten elimination, resulting in continued destruction of the villi and microvilli.
Other evidence suggests that in refractory celiac disease the cytokine interleukin 15, which is a proinflammatory cytokine, stimulates the production of interferon-gamma that may increase the attack of the intraepithelial lymphocytes against the intestinal lining in the small intestine. So, in summary it’s the T cell stimulation that doesn’t stop, that pushes interleukin 15 production, that results in the secretion of interferon gamma, which drives the intraepithelial lymphocytes against the intestine. That is actually a recipe for intestinal lymphoma.
What is the treatment for refractory celiac disease?
- Steroid therapy is the current main treatment, along with a gluten free diet of course.
- Some patients have been put on immunosuppressive drugs and even chemotherapy with cladribine has been used in a research setting.
- Some patients have been put on what is called an elemental diet which is a liquid diet that requires no digestion. It is nutrient rich with vitamins, minerals, triglycerides, amino acids. It is used to bypass all digestion and hopefully treat and or prevent malnutrition in extreme cases
- Total parental nutrition has been used as well. TPN is nutritional supplementation entirely by intravenous or non-gastrointestinal route.
- I’m in favor of identifying secondary intolerances, sensitivities and or true allergies that are most likely happening in concert. Please note this is my strong opinion as a celiac and scientist. This sadly is not the path practitioners take to address true refractory celiac disease, but it is the path I take with wonderful results.
- Arriving soon is anti-interleukin-15 monoclonal antibody which may help tame interleukin-15 for a calming impact on the immune system.