Dr. Robert Pastore, PhD, CNS
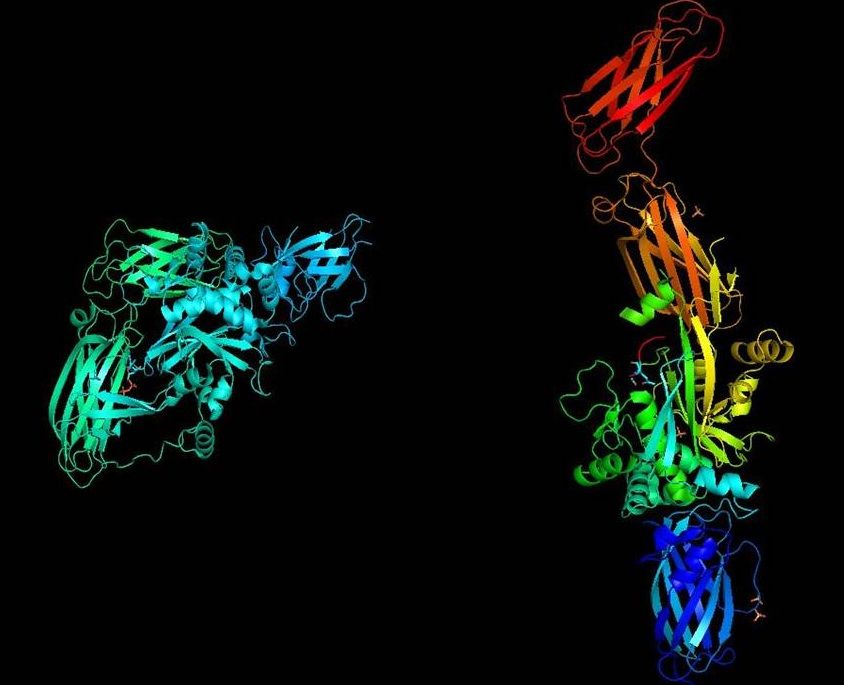
Tissue Transglutaminase
2020-05-14 • 5 min read
A biopsy of the small intestine is invasive and potentially costly depending on insurance coverage for the individual. However, here in the United states, it currently remains the gold standard for diagnosing celiac disease.
I do believe that will change in my life time and even the top gastroenterologists that believe in biopsy-based diagnosis, would love to reach a point when it is not necessary. Therefore, it is essential to have solid clinical evidence to refer a patient for a biopsy.
One excellent piece of evidence lies in what are known as antibodies toward an enzyme that can be specific in celiac disease known as anti-tissue transglutaminase antibodies (and they can be IgA and IgG).
Definition of Tissue transglutaminase
Tissue transglutaminase (also referred to as transglutaminase 2 or TTG2) is an enzyme that requires calcium for the transamidation of proteins, particularly in its association with celiac disease. In organic chemistry transamidation is the transfer of an amide group from one compound to another. The amide group is COHN2.
TTG2 is the member of a family of enzymes known as the protein-glutamine gamma-glutamyltransferases. The enzymes in this family catalyze modifications of proteins at specific side chains, crosslink lysine residues and are involved in deamidation, which in in biochemistry is the conversion of amino acid residues of glutamine and asparagine to glutamic acid or aspartic acid (other amino acids) and in organic chemistry deamidation is the conversion of an amide to a carboxylic acid (side note carboxylic acid is any organic compound with the group COOH such as fatty acids and amino acids). All these activities can result in or leave protein structures that are highly resistant to proteolysis (enzymatic protein breakdown).
Please note TTG2 is a ubiquitous enzyme and not just linked to celiac disease, but it is a crucial link in celiac disease progression. Meaning this enzyme is involved in everything from apoptotic mechanisms of cells, to cancer, to neurodegenerative diseases. It’s even found in heart muscle tissue.
TTG2 role in Celiac Pathophysiology
When a patient with celiac disease consumes gluten, it enters the submucosa in the duodenum resulting in a production of autoantibodies to tissue transglutaminase prior to the disassociation of tissue transglutaminase from the gluten molecule [1]. This changes the charge and form of the gluten molecule, promoting an autoimmune attack and fostering the binding of gluten to HLA-DQ2 and DQ8 receptors [1]. Proinflammatory cytokines including interferon-gamma are secreted into the location, along with a lymphocyte presence and gliadin specific CD 4+T cells, resulting in atrophy of the duodenal villi and microvilli[1].
Why is this the case?
In celiac disease there are two roles that are extremely important for TTG2. 1) acting as a deamindating enzyme that upregulates an immunostimulatory impact of gluten and 2) as a target autoantigen for the immune response. Keep in mind gliadin (the most toxic component of gluten for celiac disease patients is so glutamine rich) and that makes it an excellent substrate for tissue transglutaminase which results in the deamidated negatively charged peptides that will have a higher affinity for the HLA molecules (DQ2 and DQ8). Therefore, the action of TTG2 is considered a main step in celiac disease.
In the path toward diagnosis, anti-tissue transglutaminase IgA has the sensitivity and specificity over 90% in children and adults. In children the sensitivity ranges from 93.1 to 95.7% and thespecificity ranges from96.3 to 99% in adults the range for sensitivity is 90 to 95% and the specificity is 95.3 to 98.3%. Remember that the sensitivity is the ability to identify those with the disease (we call this the true positive rate) and specificity is the ability to identify those without the disease. We call this the true negative rate (vs. false negative). With that data in mind one can see why the tissue transglutaminse IgA is the cornerstone for celiac diagnosis.
What is the blood test related to TTG2?
The most common is TTG IgA. I prefer to either start with sIgA or run an sIgA in addition to the TTG IgA so that we do not miss any chance for IgA insufficiency (there is a 15-fold increase risk for sIgA deficiency in celiac disease). In the case of a selective IgA deficiency, we need to run TTG IgG and Gliadin deamidated antibody IgG (known as a DGGL blood test).
Now if the sIgA is below age-matched values then we run the TTG IGA and IGG along with DGLDN (gliadin deamidated antibodies IgG and IgA.
If the sIgA is completely normal or elevated, then we simple look at the TTG IgA results and see where they land on a scale. Using the Mayo Clinic scale as a reference, if TTG IgA is between 4.0 U/mL and 10 U/mL I do like a follow up that includes DAGL (gliadin deamidated antibody IgA) and Endomysial antibody IgA.
If the TTG igA is greater than 10 U/mL that patient should be referred directly to a biopsy.
Footnotes
- Green PH, Cellier C. Celiac disease. N Engl J Med. 2007 Oct 25;357(17):1731-43. Review. PubMed PMID: 17960014. ↩